PATIENTS SHOULD BE COUNSELED THAT THIS PRODUCT DOES NOT PROTECT AGAINST HIV INFECTION (AIDS) AND OTHER SEXUALLY TRANSMITTED DISEASES
Rx only
DESCRIPTION
MIRENA
® (levonorgestrel-releasing intrauterine system) consists of a T-shaped polyethylene frame (T-body) with a steroid reservoir (hormone elastomer core) around the vertical stem. The reservoir consists of a cylinder, made of a mixture of levonorgestrel and silicone (polydimethylsiloxane), containing a total of 52 mg levonorgestrel. The reservoir is covered by a silicone (polydimethylsiloxane) membrane. The T-body is 32 mm in both the horizontal and vertical directions. The polyethylene of the T-body is compounded with barium sulfate, which makes it radiopaque. A mono-filament brown polyethylene removal thread is attached to a loop at the end of the vertical stem of the T-body.
Inserter
MIRENA
® is packaged sterile within an inserter. The inserter, which is used for insertion of
MIRENA
® into the uterine cavity, consists of a symmetric two-sided body and slider that are integrated with flange, lock, pre-bent insertion tube and plunger. Once
MIRENA
® is in place, the inserter is discarded.
MIRENA
® is intended to provide an initial release rate of 20 µg/day of levonorgestrel.
Levonorgestrel USP, (-)-13-Ethyl-17-hydroxy-18,19-dinor-17(alpha)-pregn-4-en-20-yn-3-one, the active ingredient in
MIRENA
®, has a molecular weight of 312.4, a molecular formula of C
21
H
28
O
2
, and the following structural formula:
CLINICAL PHARMACOLOGY
Levonorgestrel is a progestogen used in a variety of contraceptive products. Low doses of levonorgestrel can be administered into the uterine cavity with the
MIRENA
® intrauterine delivery system. Initially, levonorgestrel is released at a rate of approximately 20 µg/day. This rate decreases pro-gressively to half that value after 5 years.
MIRENA
® has mainly local progestogenic effects in the uterine cavity. Morphological changes of the endometrium are observed, including stromal pseudodecidualization, glandular atrophy, a leucocytic infiltration and a decrease in glandular and stromal mitoses.
Ovulation is inhibited in some women using
MIRENA
®. In a 1-year study approximately 45% of menstrual cycles were ovulatory and in another study after 4 years 75% of cycles were ovulatory.
The local mechanism by which continuously released levonorgestrel enhances contraceptive effectiveness of the IUS has not been conclusively demonstrated. Studies of
MIRENA
® prototypes have suggested several mechanisms that prevent pregnancy: thickening of cervical mucus preventing passage of sperm into the uterus, inhibition of sperm capacitation or survival, and alteration of the endometrium.
Clinical Pharmacokinetics
Following insertion of
MIRENA
®, the initial release of levonorgestrel into the uterine cavity is 20 µg/day. A stable plasma level of levonorgestrel of 150-200 pg/mL occurs after the first few weeks following insertion of
MIRENA
®. Levonorgestrel levels after long term use of 12, 24, and 60 months were 180±66 pg/mL, 192±140 pg/mL, and 159±59 pg/mL, respectively. The plasma concentrations achieved by
MIRENA
are lower than those seen with levonorgestrel contraceptive implants and with oral contraceptives. Unlike oral contraceptives, plasma levels with
MIRENA
do not display peaks and troughs.
The mean ± SD levonorgestrel endometrial tissue concentration in four women using levonorgestrel intrauterine systems releasing 30 µg/day of levonorgestrel for 36-49 days was 808 ± 511 ng/g wet tissue weight. The endometrial tissue concentration in 2 women who had been taking a 250 ug levonorgestrel-containing oral contraceptive for 7 days was 3.5 ng/g wet tissue weight. In contrast, Fallopian tube and myometrial levonorgestrel tissue concentrations were of the same order of magnitude in the
MIRENA
® group and the oral contraceptive group (between 1 and 5 ng/g of wet weight of tissue).
The pharmacokinetics of levonorgestrel itself have been extensively studied and reported in the literature. Levonorgestrel in serum is primarily bound to proteins (mainly sex hormone binding globulin) and is extensively metabolized to a large number of inactive metabolites. Metabolic clearance rates may differ among individuals by several-fold, and this may account in part for wide individual variations in levonorgestrel concentrations seen in individuals using levonorgestrel-containing contraceptive products. The elimination half-life of levonorgestrel after daily oral doses is approximately 17 hours; both the parent drug and its metabolites are primarily excreted in the urine.
Pharmacokinetic studies of this product have not been conducted in special populations (pediatric, renal insufficiency, hepatic insufficiency, and different ethnic groups).
Drug-Drug Interactions:
The effect of other drugs on the efficacy of
MIRENA
® has not been studied.
INDICATIONS AND USAGE
MIRENA
® is indicated for intrauterine contraception for up to 5 years. Thereafter, if continued contraception is desired, the system should be replaced.
RECOMMENDED PATIENT PROFILE
MIRENA
® is recommended for women who have had at least one child, are in a stable, mutually monogamous relationship, have no history of pelvic inflammatory disease, and have no history of ectopic pregnancy or condition that would predispose to ectopic pregnancy.
Clinical Studies
MIRENA
has been studied for safety and efficacy in two large clinical trials in Finland and Sweden. In study sites having verifiable data and informed consent, 1169 women 18 to 35 years of age at enrollment used
MIRENA
® for up to 5 years, for a total of 45,000 women-months of exposure. The study population was predominantly Caucasian, and over 70% of the participants had previously used IUDs. The reported 12-month pregnancy rates were less than or equal to 0.2 per 100 women and the cumulative 5-year pregnancy rate was approximately 0.7 per 100 women. However, due to limitations of the available data, a precise estimate of the pregnancy rate is not possible.
The following table provides estimates of the percent of women likely to become pregnant while using a particular contraceptive method for one year. These estimates are based on a variety of studies. In this table,
MIRENA
® is identified as "LNg 20".
TABLE. 1--Percentage of women experiencing an unintended pregnancy during the first year of typical use and first year of perfect use of contraception and the percentage continuing use at the end of the first year. United States.
|
|
% of Women Experiencing an
Accidental Pregnancy
within the First Year of Use
|
% of Women
Continuing Use
at One Year
3
|
|
|
Typical
Use
1
(2)
|
Perfect
Use
2
(3)
|
(4)
|
|
|
85
|
85
|
|
|
|
26
|
6
|
40
|
|
|
25
|
|
63
|
|
Calendar
|
|
9
|
|
|
|
|
3
|
|
|
|
|
2
|
|
|
Post-ovulation
|
|
1
|
|
|
|
19
|
4
|
|
|
|
|
|
|
|
Parous women
|
40
|
26
|
42
|
|
Nulliparous women
|
20
|
9
|
56
|
|
|
|
|
|
|
Parous women
|
40
|
20
|
42
|
|
Nulliparous women
|
20
|
9
|
56
|
|
|
20
|
6
|
56
|
|
|
|
|
|
|
Female (Reality)
|
21
|
5
|
56
|
|
Male
|
14
|
3
|
61
|
|
|
5
|
|
71
|
|
progestin only
|
|
0.5
|
|
|
combined
|
|
0.1
|
|
|
IUD:
|
|
|
|
|
Progesterone T:
|
2.0
|
1.5
|
81
|
|
Copper T 380A
|
0.8
|
0.6
|
78
|
|
LNg 20
|
0.1
|
0.1
|
81
|
|
Depo Provera
|
0.3
|
0.3
|
70
|
|
Norplant and Norplant-2
|
0.05
|
0.05
|
88
|
|
|
0.5
|
0.5
|
100
|
|
|
0.15
|
0.10
|
100
|
|
|
1 Among
typical
couples who initiate use of a method (not necessarily for the first time), the percentage who experience an accidental pregnancy during the first year if they do not stop use for any other reason.
|
2 Among couples who initiate use of a method (not necessarily for the first time) and who use it
perfectly
(both consistently and correctly), the percentage who experience an accidental pregnancy during the first year if they do not stop use for any reason.
|
3 Among couples attempting to avoid pregnancy, the percentage who continue to use a method for one year.
|
|
|
|
|
|
|
|
|
|
|
|
CONTRAINDICATIONS
MIRENA
® insertion is contraindicated when one or more of the following conditions exist:
-
Pregnancy or suspicion of pregnancy.
-
Congenital or acquired uterine anomaly including fibroids if they distort the uterine cavity.
-
Acute pelvic inflammatory disease or a history of pelvic inflammatory disease unless there has been a subsequent intrauterine pregnancy.
-
Postpartum endometritis or infected abortion in the past 3 months.
-
Known or suspected uterine or cervical neoplasia or unresolved, abnormal Pap smear.
-
Genital bleeding of unknown etiology.
-
Untreated acute cervicitis or vaginitis, including bacterial vaginosis or other lower genital tract infections until infection is controlled.
-
Acute liver disease or liver tumor (benign or malignant).
-
Woman or her partner has multiple sexual partners.
-
Conditions associated with increased susceptibility to infections with microorganisms. Such conditions include, but are not limited to, leukemia, acquired immune deficiency syndrome (AIDS), and I.V. drug abuse.
-
Genital actinomycosis (See
WARNINGS
).
-
A previously inserted IUD that has not been removed.
-
Hypersensitivity to any component of this product.
-
Known or suspected carcinoma of the breast.
-
History of ectopic pregnancy or condition that would predispose to ectopic pregnancy.
WARNINGS
-
Ectopic Pregnancy
In large clinical trials of
MIRENA
®, half of all pregnancies detected during the studies were ectopic. The per-year incidence of ectopic pregnancy in the clinical trials was approximately 1 ectopic pregnancy per 1000 users per year. The rate of ecotopic pregnancies associated with
MIRENA
® use is not significantly different than the rate for sexually active women not using any contraception.
Clinical trials of
MIRENA
® excluded women with a history of ectopic pregnancy.
MIRENA
® is not recommended for use in women with a history of ectopic pregnancy or conditions that increase the risk of ectopic pregnancy. Women who choose
MIRENA
® must be warned about the risks of ectopic pregnancy. They should be taught to recognize and report to their physician promptly any symptoms of ectopic pregnancy. Women should also be informed that ectopic pregnancy has been associated with complications leading to loss of fertility.
-
Intrauterine Pregnancy
In the event of an intrauterine pregnancy with
MIRENA
®, the following should be considered.
-
Septic abortion
In patients becoming pregnant with an IUD in place, septic abortion-with septicemia, septic shock, and death-may occur. If pregnancy should occur with
MIRENA
® in place,
MIRENA
® should be removed. Removal or manipulation of
MIRENA
® may result in pregnancy loss.
-
Continuation of pregnancy
If a woman becomes pregnant with
MIRENA
® in place and if
MIRENA
® cannot be removed or the woman chooses not to have it removed, she should be warned that failure to remove
MIRENA
® increases the risk of miscarriage, sepsis, premature labor and premature delivery. She should be followed closely and advised to report immediately any flu-like symptoms, fever, chills, cramping, pain, bleeding, vaginal discharge or leakage of fluid.
-
Long-term effects and congenital anomalies
When pregnancy continues with
MIRENA
® in place, long-term effects on the offspring are unknown. Because of the intrauterine administration of levonorgestrel and local exposure to the hormone, the possibility of teratogenicity following exposure to
MIRENA
® cannot be completely excluded. Clinical experience with the outcomes of pregnancies is limited due to the small number of reported pregnancies following exposure to
MIRENA
®.
Congenital anomalies have occurred infrequently when
MIRENA
® has been in place during pregnancy. In these cases the role of
MIRENA
® in the development of the congenital anomalies is unknown. As of September 1999, 32 live births following exposure to
MIRENA
® were reported retrospectively. All but 2 of the infants were healthy at birth. One infant had pulmonary artery hypoplasia and another infant had cystic hypoplastic kidneys. (A sibling of this infant had renal agenesis with no
MIRENA
® exposure.)
-
exposure.
As of 1999, four cases of Group A streptococcal sepsis (GAS) out of an estimated 1.3 million
MIRENA
® users were reported. All four women experienced the symptom of severe pain within hours of insertion, and this was followed by sepsis within a few days (of insertion). All recovered with treatment. Since death from GAS is more likely if treatment is delayed, it is important to be aware of these rare but serious infections. Aseptic technique during
MIRENA
® insertion is essential. (GAS sepsis can also occur postpartum, after minor surgery, in wounds and in association with other IUDs.)
-
Pelvic Inflammatory Disease (PID)
MIRENA
® is contraindicated in the presence of known or suspected PID or in women with a history of PID unless there has been a subsequent intrauterine pregnancy. Use of IUDs has been associated with an increased risk of PID. The highest risk of PID occurs shortly after insertion (usually within the first 20 days thereafter) (see
Insertion Precautions
). A decision to use
MIRENA
® must include consideration of the risks of PID.
-
Women at increased risk for PID
PID is often associated with a sexually transmitted disease, and
MIRENA
® does not protect against sexually transmitted disease. The risk of PID is greater for women who have multiple sexual partners, and also for women whose sexual partner(s) have multiple sexual partners. Women who have ever had PID are at increased risk for a recurrence or re-infection.
-
PID warning to
MIRENA
® users
All women who choose
MIRENA
® must be informed prior to insertion about the possibility of PID and that PID can cause tubal damage leading to ectopic pregnancy or infertility, or in infrequent cases can necessitate hysterectomy, or can cause death. Patients must be taught to recognize and report to their physician promptly any symptoms of pelvic inflammatory disease. These symptoms include development of menstrual disorders (pro-longed or heavy bleeding), unusual vaginal discharge, abdominal or pelvic pain or tenderness, dyspareunia, chills, and fever.
-
Asymptomatic PID
PID may be asymptomatic but still result in tubal damage and its sequelae.
-
Treatment of PID
Following a diagnosis of PID, or suspected PID, bacteriologic specimens should be obtained and antibiotic therapy should be initiated promptly. Removal of
MIRENA
® after initiation of antibiotic therapy is usually appropriate. Guidelines for PID treatment are available from the Center for Disease Control (CDC), Atlanta, Georgia. Adequate PID treatment requires the application of current standards of therapy prevailing at the time of occurrence of the infection with reference to prescription labeling.
Actinomycosis has been associated with IUDs. Symptomatic women with IUDs should have the IUD removed and should receive antibiotics. However, the management of the asymptomatic carrier is controversial because actinomycetes can be found normally in the genital tract cultures in healthy women without IUDs. False positives findings of actinomycosis on Pap smears can be a problem. When possible, confirm the Pap smear diagnosis with cultures.
-
Irregular Bleeding and Amenorrhea
MIRENA
® can alter the bleeding pattern. During the first three to six months of
MIRENA
® use the number of bleeding and spotting days may be increased and bleeding patterns may be irregular. Thereafter, the number of bleeding and spotting days usually decreases but bleeding may remain irregular. If bleeding irregularities develop during prolonged treatment, appropriate diagnostic measures.should be taken to rule out endometrial pathology.
Amenorrhea develops in approximately 20% of
MIRENA
® users by one year. The possibility of pregnancy should be considered if menstruation does not occur within six weeks of the onset of previous menstruation. Once pregnancy has been excluded, repeated pregnancy tests are not necessary in amenorrheic subjects unless indicated by other signs of pregnancy or by pelvic pain.
-
Embedment
Partial penetration or embedment of
MIRENA
® in the myometrium may decrease contraceptive effectiveness and can result in difficult removals.
-
Perforation
An IUD may perforate the uterus or cervix, most often during insertion although the perforation may not be detected until some time later. If perforation occurs, the IUD must be removed and surgery may be required. Adhesions, peritonitis, intestinal perforations, intestinal obstruction, abscesses and erosion of adjacent viscera have been reported with IUDs.
It is recommended that postpartum
MIRENA
® insertion be delayed until uterine involution is complete to decrease perforation risk. There is an increased risk of perforation in women who are lactating. Inserting
MIRENA
® immediately after first trimester abortion is not known to increase the risk of perforation, but insertion after second trimester abortion should be delayed until uterine involution is complete.
-
Ovarian Cysts
Since the contraceptive effect of
MIRENA
® is mainly due to its local effect, ovulatory cycles with follicular rupture usually occur in women of fertile age using
MIRENA
®. Sometimes atresia of the follicle is delayed and the follicle may continue to grow. Enlarged follicles have been diagnosed in about 12% of the subjects using
MIRENA
®. Most of these follicles are asymptomatic, although some may be accompanied by pelvic pain or dyspareunia. In most cases the enlarged follicles disappear spontaneously during two to three month's observation. Surgical intervention is not usually required.
-
Breast cancer
Women who currently have or have had breast cancer should not use hormonal contraception because breast cancer is a hormone-sensitive tumor.
-
Risks of Mortality
The available data from a variety of sources have been analyzed to estimate the risk of death associated with various methods of contraception. The estimates of risk of death include the combined risk of the contraceptive method plus the risk of pregnancy or abortion in the event of method failure. The findings of the analysis are shown in Table 2.
Table 2--Annual Number of Birth-Related or Method-Related Deaths Associated with Control of Fertility per 100,000 Nonsterile Women, by Fertility Control Method According to Age
|
|
AGE GROUP
|
|
METHODS
|
15-19
|
20-24
|
25-29
|
30-34
|
35-39
|
40-44
|
|
|
4.7
|
5.4
|
4.8
|
6.3
|
11.7
|
20.6
|
|
|
2.1
|
2.0
|
1.6
|
1.9
|
2.8
|
5.3
|
|
IUD
|
0.2
|
0.3
|
0.2
|
0.1
|
0.3
|
0.6
|
|
|
1.4
|
1.3
|
0.7
|
1.0
|
1.0
|
1.9
|
|
|
0.9
|
1.7
|
0.9
|
1.3
|
0.8
|
1.5
|
|
|
0.6
|
1.2
|
0.6
|
0.9
|
0.5
|
1.0
|
|
Diaphragm/Cap
|
0.6
|
1.1
|
0.6
|
0.9
|
1.6
|
3.1
|
|
|
0.8
|
1.5
|
0.8
|
1.1
|
2.2
|
4.1
|
|
Spermicides
|
1.6
|
1.9
|
1.4
|
1.9
|
1.5
|
2.7
|
|
|
0.8
|
1.3
|
1.1
|
1.8
|
1.0
|
1.9
|
|
Implants/Injectables
|
0.2
|
0.6
|
0.5
|
0.8
|
0.5
|
0.6
|
|
|
1.3
|
1.2
|
1.1
|
1.1
|
1.2
|
1.3
|
|
|
0.1
|
0.1
|
0.1
|
0.1
|
0.1
|
0.2
|
Harlap S. et al., Preventing Pregnancy, protecting health: a new look at birth control choices in the US. The Alan Guttmacher Institute 1991: 1-129.
|
|
PRECAUTIONS
PATIENTS SHOULD BE COUNSELED THAT THIS PRODUCT DOES NOT PROTECT AGAINST HIV INFECTION (AIDS) AND OTHER SEXUALLY TRANSMITTED DISEASES.
1. Patient Counseling
Prior to insertion, the physician, nurse, or other trained health professional must provide the patient with the Patient Package Insert. The patient should be given the opportunity to read the information and discuss fully any questions she may have concerning
MIRENA
® as well as other methods of contraception.
Careful and objective counseling of the user, prior to insertion, regarding the expected bleeding pattern, the possible interindividual variation in changes in bleeding and the etiology of the changes may have an effect on the frequency of removal due to bleeding problems and amenorrhea.
The patient should be told that some bleeding such as irregular or prolonged bleeding and spotting, and/or cramps may occur during the first few weeks after insertion. If her symptoms continue or are severe she should report them to her health care provider. She should also be given instructions on what other symptoms require her to call her physician. She should be instructed on how to check after her menstrual period to make certain that the thread still protrudes from the cervix and cautioned not to pull on the thread and displace
MIRENA
®. She should be informed that there is no contraceptive protection if
MIRENA
® is displaced or expelled.
Patient Evaluation and Clinical Considerations
-
A complete medical and social history, including that of the partner, should be obtained to determine conditions that might influence the selection of an IUD for contraception (see
CONTRAINDICATIONS
). A physical examination should include a pelvic examination, a Pap smear, and appropriate tests for any other forms of genital disease, such as gonorrhea and chlamydia laboratory evaluations, if indicated.
Special attention must be given to ascertaining whether the woman is at increased risk of ectopic pregnancy or PID. MIRENA® is contraindicated in these women.
-
The health care provider should determine that the patient is not pregnant.
The possibility of insertion of
MIRENA
® in the presence of an existing undetermined pregnancy is reduced if insertion if performed within 7 days of the onset of a menstrual period.
MIRENA
® can be replaced by a new system at any time in the cycle.
MIRENA
® can be inserted immediately after first trimester abortion.
-
MIRENA
® should not be inserted until 6 weeks postpartum or until involution of the uterus is complete in order to reduce the incidence of perforation and expulsion.
-
Patients with certain types of valvular or congenital heart disease and surgically constructed systemic-pulmonary shunts are at increased risk of infective endocarditis. Use of
MIRENA
® in these patients may represent a potential source of septic emboli. Patients with known congenital heart disease who may be at increased risk should be treated with appropriate antibiotics at the time of insertion and removal. Patients requiring chronic corticosteroid therapy or insulin for diabetes should be monitored with special care for infection.
-
MIRENA
® should be used with caution in patients who have a coagulopathy or are receiving anticoagulants.
-
Use of
MIRENA
® in patients with vaginitis or cervicitis should be postponed until proper treatment has eradicated the infection and until it has been shown that the cervicitis is not due to gonorrhea or chlamydia (see
CONTRAINDICATIONS
).
2. Insertion Precautions
Because the presence of organisms capable of establishing PID cannot be determined by appearance, and because IUD insertion may be associated with introduction of vaginal bacteria into the uterus, strict asepsis should be observed at insertion. Administration of antibiotics may be considered, but the utility of this treatment is unknown.
The uterus should be carefully sounded prior to
MIRENA
® insertion to determine the degree of patency of the endocervical canal and the internal os, and the direction and depth of the uterine cavity. In occasional cases, severe cervical stenosis may be encountered. Do not use excessive force to overcome this resistance.
Syncope, bradycardia, or other neurovascular episodes may occur during insertion or removal of MIRENA, especially in patients with a predisposition to these conditions or cervical stenosis. If decreased pulse, perspiration, or pallor are observed, the patient should remain supine until these signs have disappeared.
3. Continuation and Removal
MIRENA
® must be replaced every 5 years because contraceptive effectiveness after 5 years has not been established
-
User complaints of pain, odorous discharge, bleeding, fever, genital lesions or sores should be promptly responded to and prompt examination recommended. (See Warnings regarding amenorrhea).
-
If examination during visits subsequent to insertion reveals that the length of the threads has changed from the length at time of insertion, and the system is verified as displaced, it should be removed. A new system may be inserted at that time or during the next menses if it is certain that conception has not occurred. If the threads are not visible, location of the
MIRENA
® should be verified, for example with X-ray, ultrasound, or gentle probing of the uterine cavity. If the
MIRENA
® is in place with no evidence of perforation, no intervention is indicated. If expulsion has occurred, it may be replaced within 7 days of a menstrual period after pregnancy has been ruled out.
-
Since
MIRENA
® may be displaced, patients should be reexamined and evaluated shortly after the first postinsertion menses, but definitely within 3 months after insertion. Symptoms of the partial or complete expulsion of any lUD may include bleeding or pain. However, the system can be expelled from the uterine cavity without the woman noticing it. Partial expulsion may decrease the effectiveness of
MIRENA
®. As menstrual flow usually decreases after the first 3 to 6 months of
MIRENA
® use, increase of menstrual flow may be indicative of an expulsion.
-
In the event a pregnancy is confirmed during
MIRENA
® use, the following steps should be taken:
-
Determine whether pregnancy is ectopic and take appropriate measures if it is.
-
Inform patient of the risks of leaving
MIRENA
® in place or removing it during pregnancy and of the lack of data on long-term effects on the offspring of women who have had
MIRENA
® in place during conception or gestation (see WARNINGS ).
-
If possible,
MIRENA
® should be removed after the patient has been warned of the risks of removal. If removal is difficult, the patient should be counseled and offered pregnancy termination.
-
If
MIRENA
® is left in place, the patient' course should be followed closely.
-
Should the patient' relationship cease to be mutually monogamous, or should her partner become HIV positive, or acquire a sexually transmitted disease, she should be instructed to report this change to her clinician immediately. The use of a barrier method as a partial protection against acquiring sexually transmitted diseases should be strongly recommended. Removal of
MIRENA
® should be considered.
-
MIRENA
® should be removed for the following medical reasons: menorrhagia and/or metrorrhagia producing anemia; acquired immune deficiency syndrome (AIDS); sexually transmitted disease; pelvic infection; endometritis; symptomatic genital actinomycosis; intractable pelvic pain; severe dyspareunia; pregnancy; endometrial or cervical malignancy; uterine or cervical perforation.
-
If the retrieval threads are not visible, they may have retracted into the uterus or have been broken, or
MIRENA
® may have been broken, perforated the uterus, or have been expelled. Location of
MIRENA
® may be determined by sonography, X-ray, or by gentle exploration of the uterine cavity with a probe.
-
Removal of the system should also be considered if any of the following conditions arise for the first time:
4. Glucose Tolerance
Levonorgestrel may affect glucose tolerance, and the blood glucose concentration should be monitored in diabetic users of
MIRENA
®.
The effect of hormonal contraceptives may be impaired by drugs which induce liver enzymes. The influence of these drugs on the contraceptive efficacy of
MIRENA
® has not been studied.
CARCINOGENESIS
Long-term studies in animals to assess the carcinogenic potential of levonorgestrel releasing intrauterine system have not been performed. See
WARNINGS
section.
PREGNANCY
Pregnancy Category X. See
WARNINGS
section.
NURSING MOTHERS
Levonorgestrel has been identified in small quantities in the breast milk of lactating women using
MIRENA
®. In a study of 14 breastfeeding women using a
MIRENA
® prototype during lactation, mean infant serum levels of levonorgestrel were approximately 7% of maternal serum levels. Hormonal contraceptives are not recommended as the contraceptive method of first choice during lactation.
PEDIATRIC USE
Safety and efficacy of
MIRENA
® have been established in women of reproductive age. Use of this product before menarche is not indicated. (See
RECOMMENDED PATIENT PROFILE
)
GERIATRIC USE
MIRENA
® has not been studied in women over age 65 and is not currently approved for use in this population.
INFORMATION FOR THE PATIENT (See Patient Labeling)
Patients should also be advised that the prescribing information is available to them at their request. It is recommended that potential users be fully informed about the risks and benefits associated with the use of
MIRENA
®, with other forms of contraception, and with no contraception at all.
Return to Fertility
About 80 % of women wishing to become pregnant conceived within 12 months after removal of
MIRENA
®.
ADVERSE REACTIONS
The most serious adverse reactions associated with the use of
MIRENA
® are discussed above in the Warnings section. Others are presented in the Precautions section. Other adverse events reported by 5% or more subjects include:
Abdominal pain
Leukorrhea
Headache
Vaginitis
Back pain
Breast pain
Acne
Depression
Hypertension
Upper respiratory infection
Nausea
Nervousness
Dysmenorrhea
Weight increase
Skin disorder
Decreased libido
Abnormal Pap smear
Sinusitis
Other reported adverse reactions occurring in less than 3% of patients include: failed insertion, migraine, vomiting, anemia, cervicitis, dyspareunia, hair loss, eczema.
HOW SUPPLIED
MIRENA
® (levonorgestrel-releasing intrauterine system), containing a total of 52 mg levonorgestrel, is available in a carton of one sterile unit NDC# 50419-421-01. Each
MIRENA
® is packaged in a thermoformed blister package with a peelable lid, together with an insertion tube which is then heat sealed into a secondary pouch.
MIRENA
® is supplied sterile.
MIRENA
® is sterilized with ethylene oxide. Do not resterilize. For single use only. Do not use if the inner package is damaged or open. Insert before the month shown on the label.
STORAGE AND HANDLING
Store at 25°C (77°F); with excursions permitted between 15°-30°C (59°-86°F) [See USP Controlled Room Temperature]
DIRECTIONS FOR USE
NOTE: Health care providers are advised to become thoroughly familiar with the insertion instructions before attempting insertion of
MIRENA
®.
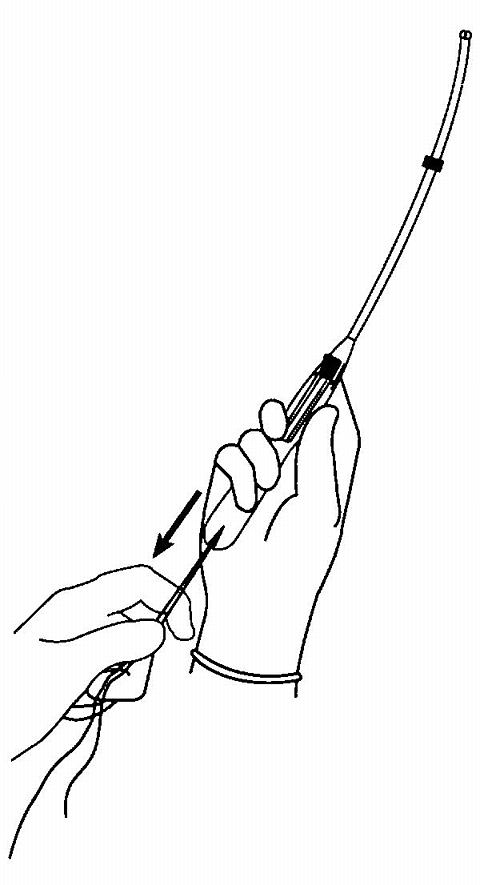
Insertion Instructions
MIRENA
® is inserted with the provided inserter (figure 1) into the uterine cavity within seven days of the onset of menstruation or immediately after first trimester abortion by carefully following the insertion instructions. It can be replaced by a new system at any time during the menstrual cycle.
Figure 1.
MIRENA® and Inserter
Preparation for insertion
Insertion Procedure
-
-
Open the sterile package.
-
Place sterile gloves on your hands.
-
Pick up the inserter containing
MIRENA
®.
-
Carefully release the threads from behind the slider, so that they hang freely.
-
Make sure that the slider is in the furthest position away from you (positioned at the top of the handle nearest the IUS).
-
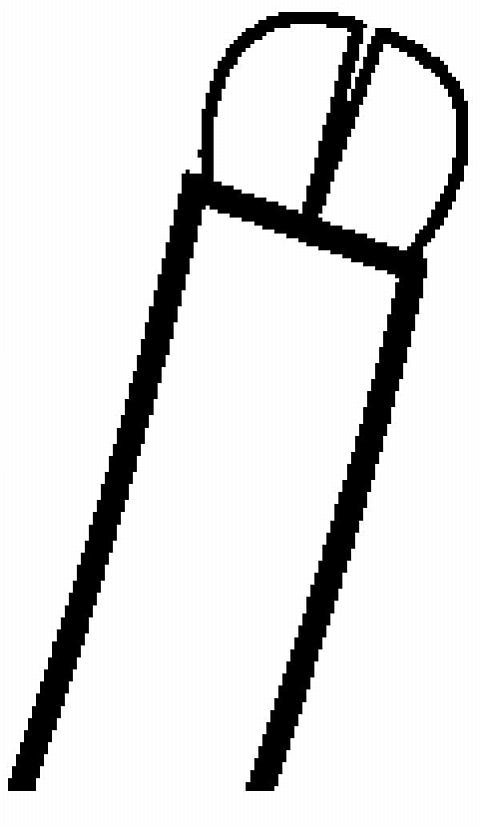
While looking at the insertion tube, check that the arms of the system are horizontal. If not, align them on a sterile surface (figure 2) or with sterile gloved fingers.
figure 2.
Checking that the arms of the system are horizontal
-
-
Pull on both threads to draw the
MIRENA
® system into the insertion tube (figure 3a).
-
Note that the knobs at the end of the arms now cover the open end of the inserter (figure 3b).
figure 3a.
MIRENA® system being drawn into the insertion tube
figure 3b.
The knobs at the ends of the arms
-
Fix the threads tightly in the cleft at end of the handle (figure 4).
figure 4.
Threads are fixed tightly in the cleft
-
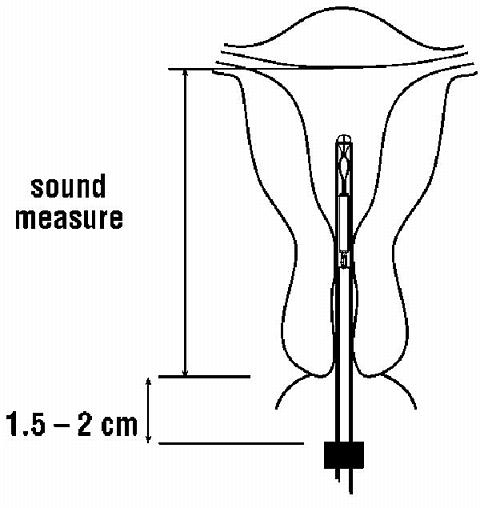
Set the flange to the depth measured by the sound, as indicated in figure 5.
figure 5.
The sound measure
-
MIRENA
® is now ready to be inserted.
Hold the slider firmly in the furthermost position (at the top of the handle). Grasp the cervix with the tenaculum and apply gentle traction to align the cervical canal with the uterine cavity. Gently insert the inserter into the cervical canal and advance the insertion tube into the uterus until the flange is situated at a distance of about 1.5-2 cm from the external cervical os to give sufficient space for the arms to open (figure 6).
NOTE! Do not force the inserter.
Figure 6.
Flange adjusted to sound depth
-
While holding the inserter steady release the arms of
MIRENA
® (figure 7a) by pulling the slider back until the top of the slider reaches the mark (raised horizontal line on the handle) (figure 7b).
figure 7a.
The arms of the MIRENA® being released
figure 7b.
Pulling the slider back to reach the mark
-
Push the inserter gently into the uterine cavity until the flange touches the cervix.
MIRENA
® should now be in the fundal position (figure 8).
figure 8.
MIRENA® in the fundal position
-
Holding the inserter firmly in position release
MIRENA
® by pulling the slider down all the way. The threads will be released automatically (figure 9).
figure 9.
Releasing MIRENA® and withdrawing the inserter
-
Remove the inserter from the uterus. Cut the threads to leave about 2-3 cm visible outside the cervix (figure 10). figure 10.
figure 10.
cutting the threads
IMPORTANT!
If you suspect that the system is not in the correct position, check placement, (with ultrasound, for example). Remove the system if it is not positioned completely within the uterus. Do not reinsert a removed system.
REMOVAL OF MIRENA®
Remove
MIRENA
® by applying gentle traction on the threads with forceps. The arms of the system will fold upward as it is withdrawn from the uterus. The system should not remain in the uterus after 5 years.
SPECIAL NOTES IF A PATIENT WANTS TO CONTINUE CONTRACEPTION AFTER REMOVAL
You may insert a new
MIRENA
® immediately following removal.
If a patient with regular cycles wants to start a different birth control method, remove the system during the first 7 days of the menstrual cycle and start the new method.
If a patient with irregular cycles or amenorrhea wants to start a different birth control method, or if you remove the system after the seventh day of the menstrual cycle, start the new method at least 7 days before removal.
© 2000, Berlex Laboratories, Inc.
www.mirena.com
All rights reserved.
6073000 12/00
Manufactured for:
Berlex Laboratories
Montville, New Jersey 07045
Manufactured in Finland
PRODUCT PHOTO(S):
NOTE: These photos can be used only for identification by shape, color, and imprint. They do not depict actual
or relative
size.
The product samples shown here have been supplied by the manufacturer and reproduced in full color by PDR as a quick-reference identification aid. While every effort has been made to assure accurate reproduction, please remember that any visual identification should be considered preliminary. In cases of poisoning or suspected overdosage, the drug' identity should be verified by chemical analysis.
Copyright© 2002 Medical Economics